-
About brain injury
-
For individuals
- Types of brain injury
-
Effects of brain injury
- Behavioural effects of brain injury
- Cognitive effects of brain injury
- Coma and reduced awareness states
- Communication problems
- Emotional effects of brain injury
- Executive dysfunction
- Fatigue after brain injury
- Hormonal imbalances
- Memory problems
- Physical effects of brain injury
- Post-traumatic amnesia
- Hospital treatment and early recovery
- Rehabilitation and continuing care
- Practical issues
- Relationships after brain injury
- Caring
- Information library
- Free training for brain injury survivors
-
Brain injury and me
- "But you don't look disabled"
- Shana Lewis
- Robert Ashton
- Laura Bailey 2015
- Jane Allberry
- Michaela
- Ian Litchfield
- Debi Pullen
- David Thomas
- Alison Winterburn
- Mel Lightfoot
- Annette Henry
- Denise Johnson
- Codey Sharp
- Keith Emmanuel
- Lizzie Smart
- Gwen and Natalie Milham
- Terisha Burge
- Maria Knights
- Joanne Davis
- Sarah Whitchurch
- Amy Perring
- Jane Clarke
- Peter Holmes
- Luke Flavell
- Lindsay Lapham
- Pip Taylor
- Nic O'Leary
- Angus Swanson
- Tom Birch
- Samuel Bishop
- Phil Broxton
- Nell Gregory
- Jamie Gailer
- Kate and John Bosley
- Gary Winters
- Kathryn Edgington
- Charlie and Jake Korving
- Bruno Muratori
- Kerry Jeffs
- Mike McCall
- James Piercy
- Andy Nicholson
- Warren McKinlay
- Lauren and Claire Cowlishaw
- Sarah McKinlay
- David Horner
- Arthur Moore
- Mike Palmer
- Sarah Tomlinson
- Paul Leyland
- Tina Young
- Warwick Jarvis
- Jackie and John Mills
- Adrian Ellis
- Kieran Wallis
- Eleanor Simcox
- Jack Rutter
- Jan Luxton
- Daniel Lingard
- Bernie Bambury
- Lorraine and Kevin Pratt
- Paul Pugh
- Melanie Whittaker
- Naomi
- John Holbrook
- Tom Wright
- Jackie Alton
- Irvine Phair
- Rebecca Grant
- Rachel Atkinson
- Marco Gambi
- Brenda and Julian
- Callum Maclean
- A simple solution
- Lost in a crowd
- Caring for carers
- Dear my new brain
- Holiday from brain injury
- The new me and my Jumbledbrain blog
- The old me is not the new me
- I see Headway as the pit stop
- Riding my horse Johnny keeps me focused
- Headway is a haven
- Brain injury didn't steal my future
- Never give up
- Anna Khan
- Fiona Grant-MacDonald
- Kiran Higgins
- Jetting off alone
- Dad 2.0
- Dislabeled
- Matt Brammeier
- Syreeta
- Brain injury vs family
- The Face of Brain Injury With Dee Snider
- Mourning lost relationships
- A mother's perspective
- Pathological laughter - it's no joke
- HiddenInMe
- Polly Williamson
- Writing a book after brain injury
- Michael Mabon
- Jeff Mayle
- A day in the life of a carer
- "Kerry the HATS nurse was my guardian angel"
- Don't struggle alone
- Harriet Barnsley
- I don't want anyone to feel as alone as I did
- Amanda Horton
- Jeff Clare
- A helping hand
- Donnie McHarg
- Shona Green
- Jenny Joppa
- Philippa Taylor
- Debra Jones
- John Dougan
- "No memory of the day that changed my life"
- Nick Gibbs
- Jean Parker
- My experience of parenting after brain injury
- Sue McIntyre
- Daniel Mole
- Keely McGhee
- Paula Stanford
- Relationships after brain injury – Imogen’s story
- Jules Pring
- Tara Moore
- Dr Amy Izycky's Headway Exhibition
- Nicola Brown
- Rod Maxwell
- Joy Webb
- Grace Vobe
- Doing it the Head way
- Carer vacancy. Unpaid. Full time. No experience required.
- Joe Sandford
- My Brain Injury ID Card
- Matthew Nichols
- Heather Pollard
- Danielle
- Noelle Robinson
- Giles Hudson
- Q&A - ‘Be in the moment. This is all you have.’
- Q&A – “I would be the Happiness Fairy, I’ve sprinkled Happy Dust on you, now smile.”
- Nature's Way: Gardening after brain injury
- The debilitating impact of social isolation
- Joanne Wood - Who
- David Greer
- Lynne O'Grady
- Clair Bennett
- Danielle's story - returning home
- Anne Johnston
- Q&A: Cat
- How I overcame panic attacks
- Q&A with Zalehka Price-Davies
- Philippa-Anne Dewhirst
- After my brain injury I kept questioning, 'what if I have lost my ability to be creative?'
- Chris Bryant
- Busting the myths around brain injury and sex
- I swear, he knew he was helping me
- Hannah Brandon
- Keith Poultney
- Joanna Darmody
- Terry Slade
- Tamara Bond
- Kavita Basi
- Nigel Limb
- Learning to live again
- David Wheeler
- Jessica Stevens
- Andrew Plowright
- Steve Borland
- Tracey Cox
- Financial fraud: a risk you can't afford to ignore
- Dating after brain injury
- Max Muteliso
- Q&A: Roger Merriman
- Parenting with a brain injury
- Ben Clench
- Kieran Broadfield
- Max Munro
- Louise Lane
- Adam Nicke - Q&A
- Hitting the High Street at Headway's Hinckley shop
- Hitting the high street at headway hinckley
- London Marathon Runners
- Rebecca Hutchings
- Joanne Wood
- Paws for Thought
- Jake Elliott
- Growing Together with Headway Cambridgeshire
- Lauren Walkington Q&A
- Daniel Parslow
- Alex Murphy
- Matt Masson
- Alphabet Brains
- Pete Bourne
- David Yabbacome
- Julie Sadler
- Lottie Butler
- Candice Ridley
- Belinda Medlock
- Unravelling the mystery of fatigue
- Lara Newson: Head Smash
- Robert Courtnell
- Hipatia Preis
- Stewart Gray
- Mary's Story
- Hannah O'Dowd
- Victoria Wicks
- Carol Smith
- ABI Week across the UK
- Rebecca Ivatts
- Nicola Evans
- 'Writing gives me meaning'
- The perils of gambling after brain injury
- Fit for purpose: The benefits of being active after brain injury
- Festival fun after brain injury
- 6 strategies for getting back to work after brain injury
- Matt Rhodes
- Clare Hull
- Stop the bus! A guide to public transport
- Maria Munn
- Brain injury: To tell or not to tell?
- 5 ways to cope with taste and smell problems after brain injury
- The uneasy relationship between alcohol and brain injury
- 9 ways to help with planning problems after brain injury
- 7 top tips for managing visual problems after brain injury
- 10 ways to cope with depression after brain injury
- Supporting children: visiting a parent in hospital
- Supporting children after a parent's brain injury: when a parent comes home
- Donna Siggers
- How to manage memory problems after brain injury
- Hot weather after brain injury: tips for keeping cool
- Stefan Leader
- Keith
- A picture speaks a thousand words
- Andrew Purnell
- Ruth Berkoff
- Sam Hulse
- Katherine McKinstry
- Chloé Briffa
- Socialising after brain injury
- Shane Booth
- Theme parks: accessibility after brain injury
- William Windle
- Ron Gains
- Rebecca Jones
- Sarah Scott
- Pregnancy after brain injury
- Music after brain injury
- Emma Martins
- Dancing after brain injury
- Scottie Elliott
- Let's talk tech
- Lorna Lancaster
- Carol Evans
- John Wrathall
- Fiona Baker-Holden
- Ryan Goodenough
- Christmas after brain injury
- Cecilia Danielsson
- Rik Waddon
- Saturday Night Fever
- Anthony Hewson
- Q&A: Julian Earl
- Fireworks after brain injury
- Coping with Christmas in hospital
- Eleanor Brander
- Beccy Young
- Veronica Woods
- 10 things not to say to someone with a brain injury
- Tracey Newman
- Lauren Gilligan
- Louis McGuire
- Fighting the bear
- David Macdonald
- Yvette Lumley
- Christina Sweeney
- Charlotte Warhurst
- Cindy Hollingsworth
- Spencer Senior
- Q&A: Steven Kelly
- Sarah Lane
- I am a firm believer in not just speaking of the change, but actively searching to be part of it.
- Carwyn Wooldridge
- Liz Wilson
- Lucy Rogoff
- Bryony Wilshaw
- David Wozny
- Sarah Allwood
- Leah Moore
- "We're all going on an assisted holiday"
- Anne's top tips for self-isolation
- Sammy's top tips for managing mental health problems during self-isolation
- Kavita's tips for self-isolation
- Belinda’s story: Isolation after brain injury
- Mikey Smithson
- Lucie Bell
- Let’s talk continence problems after brain injury
- Mark Kennedy
- Gary Younge
- Mindfulness and me
- Life in lockdown: Alison's story
- John Beaumont
- Catherine Erdal
- CinderZ
- Lyndsey Anderson
- Rock painting by Deborah Johnston
- Q&A: Hollie-Blue Huntsman
- Donna Davies
- Caroline Spiers
- Phil Birch
- More than my brain injury: Danielle Grant
- Brain Injury Sunblock and the Infernal Birdsong
- Sandra Liddell
- Brain Injury And Covid: Jane Hallard
- Brain Injury And Covid: Jean Parker
- A day in the life of a Headway helpline consultant
- Brain injury and Covid: Tom Harris
- Brain Injury And Covid: Michael Perry
- Rebekah Nesbitt
- The Headway helpline: You're not alone
- The price of a punch
- David Baker
- Donna Harris
- 7 signs of executive dysfunction after brain injury
- My poetry: Joseph McAloon
- Angela Lewis
- Daniel Sutherland
- Andrew Brown
- Sarah McGrath
- Dan Goldstraw
- In her own words: Emma Davey
- My poetry: John Marshall
- Disinfectant by Sarah-Louise Lennon
- Karen Whitehead
- Wendy Joss
- In his own words: Max Bongard
- Karl Hargreaves
- Animation: Memory loss after brain injury
- How to cope with memory problems after brain injury
- Q&A: George Mitchell
- Michelle Hay
- Q&A: Alan Heal
- Lucy Hunter
- Cara's story
- Q&A: Rosemary Shaw
- Mental health and brain injury
- Emma Chivers
- Q&A: Terence Berritt
- Q&A: Emma Linnell
- Tai Chi After Brain Injury with Dr Giles Yeates
- In her own words: Emma Lindsay
- Phillip Cragg
- Paintings by Hannah Jenkins
- Q&A: Alison Rockall
- Imogen Cauthery
- Alex Danson-Bennett MBE
- My poetry: Helen Wilson
- Haydn Garrod
- Podcast: Life with no filter
- Overcoming challenges after brain injury
- Creative Expression: Mark and Jules Kennedy
- Eleanor Furneaux
- Creative Expression: Lucy Pugh
- Claire Bullimore
- My artwork: Sandra E Ball
- Blue Mundane Monday Mix by Glen Stephenson
- Nicola Cross
- Survival is a Team Dream by Philippa Bateman
- Brain Attack Music by Andy Dovey
- Top tips for coping with parenting through lockdown
- Pauline O'Connor
- Duncan Boak
- Gill and Terry Oliver
- Jelly Brain documentary: A gift to mum
- In her own words: Jodie Bacon
- Monica Petrosino
- Josh Rawson
- What triggers anger after brain injury?
- Gerald Heffernan
- Back behind the wheel: Paula Barlow
- Back behind the wheel: Driving FAQs
- Elizabeth Wilkins
- My poetry: Sam Norris
- Alex Richardson
- Emerging from lockdown: Tips for brain injury survivors
- My podcast by Nikki Webber MBE
- Isolation and loneliness: Life with no filter podcast
- A life of lockdown? Belinda's story
- A life of lockdown? Derek's story
- A life of lockdown? Melanie's story
- A life of lockdown? Elizabeth's story
- Mindfulness Training after Brain Injury with Dr Niels Detert
- Fresh Start by the Headway Glasgow Writing Group
- 'I've Made It!' by Becki York
- Lucy O'Donovan
- Top tips for coping with headaches
- Helena Breslin
- Sue Williams
- Reflections of Chair-Man Eason
- Ceara's story
- Tracy Dickson
- Julie Mueller
- Thomas Leeds
- Headaches: The whats, whys and hows
- My photography: Rob Dinwoodie
- Nick Henderson
- Lenka Brunclikova
- Emma Doherty
- Planting a seed of thought - Natalie Parr
- 'My Broken Brain' by Sam Hedges
- Sally Smith
- Catherine Jessop - Pulling Through
- Helen Bray
- Exploring your dreams
- Sweet dreams? Getting a good night's sleep after brain injury
- Mindfulness after brain injury
- Mike Clark
- Amy Streather
- Eleanor May Blackburn
- Paul Wilkins
- Barry Cusack: My body and mind
- Our relationship reality: Love after brain injury
- Love after brain injury: Thalia and Matt
- Tisha's story
- Executive dysfunction explained
- Let’s talk about sex...
- When Catwalks are Barbed
- Hope by Angela Webb
- Dee Gall
- Headway gets creative!
- From a child's mind to centre stage
- Bernadette Bendall
- Zoe Rainaki
- What did you not see? By Stef Harvey
- A Windy Moment by Nick Fletcher
- Helen and Liz
- The Sound of Recovery
- A family united to support life after brain injury
- See the Hidden Me: Iona's story
- See the Hidden Me: Annette's story
- See the Hidden Me: John's story
- See the Hidden Me: Christine's story
- The Brain Injury Cookbook
- Raj Gataora
- Marco Gambi: A passion for food
- Celebrating 10,000 Brain Injury ID Cards
- 'Rehabilitation rather than incarceration'
- Theresa Malcom
- Tim Richens
- Visual problems: A closer look
- Dusty Zeisberger – 24-hour treadmill challenge
- A conversation with... Ian Scott-Logan
- Ways to help cope at Christmas: tips for survivors, families, friends, and carers
- Lisa
- Bryce Bell
- World’s first ABI Games a huge success!
- Steven Lomas
- Memory systems
- Stevie Ward
- Five Years On by Clare Jones
- The Penny Drops
- Stephen Evans
- Don’t get bitten by the sharks!
- Jonathan Hirons
- Finding your superpower...
- Post-traumatic growth after brain injury
- Nick Blackwell
- Heads, Hats and Healing: Making and Creating Silver Linings
- Nigel and Paula's story
- Joseph's story
- John's story
- How to manage isolation after brain injury
- Managing anxiety after brain injury
- Simon and Marc's story
- Sandi's story
- Relearning life skills
- "A charity of love"
- Dawn, Headway volunteer
- Pat Griffiths, Chair of Trustees for Headway Meirionnydd
- Creative writing sessions: Laura Bailey
- Creative writing sessions: Helen Davies
- Nicola Bird Blunt
- In her own words: Lynn Boyle
- My brother was killed by one punch: Aaron Matcham
- Completing my life-long dream of running the Brighton Marathon: Adam Clarke
- 8 ways to manage a lack of insight after brain injury
- How to help someone with a brain injury: Top tips for friends and family
- Balance problems after brain injury
- Safe travels! Your holiday tips
- Early warning signs of fatigue
- Keeping your relationship healthy after brain injury
- Carers: Try these 4 ways to care for yourself
- 7 tips for volunteering after brain injury
- 10 top tips for coping with stress after brain injury
- Top 10 tips for staying safe online
- In memory of much-loved partner and dad
- 10 ways to manage anger: tips for brain injury survivors
- Managing impulsivity and disinhibition following brain injury
- Friends: 5 ways to support someone with a brain injury
- Diet after brain injury: Healthy body, healthy mind?
- Top tips for a good night's sleep
- An awfully big row: Giles Johnson
- Jurate Ardour
- Dean Osborne
- Errol
- Iain Millar: Rising from Adversity to Find Purpose on the Golf Course
- Finding Hope on the Fairway, Anthony Roberts' Journey of Resilience and Inspiration
- Ben Fowler
- James Heather
- Andy Southey
- From one punch victim to Headway Hero: A Half Marathon triumph
- Mark Winterbourne
- World Mental Health Day
- Thanking Our Fundraiser: Sahara Trek Triumphm
- Sisters’ challenge inspired by ‘hero’ sibling’s brain injury
- Ed Dunford
- The devastating consequences of one punch
- Get to know – Jen, Director of Fundraising
- Putting the ‘I’ in identity after brain injury
- Coping with winter blues
- Making returning to work, work for you
- Alan's story
- Get to know – Sarah, Trust and Foundations Manager
- Give up, or focus tremendously on rehabilitation
- What really counts?
- Laura Macfarlane
- The role art can play in positive change
- World Poetry Day
- Poem: TBI Survivor
- Adapting to life after brain injury: Returning to work
- Meet the volunteer - Roger Beattie
- We are family! Siblings run for Headway in support of their mum
- The impact of brain injury on a family
- A craniotomy – ‘the last resort’
- David's story A Life Re-written
- Andrew's story A Life Re-written
- Alison's story A Life Re-written
- Liz and Justina's story A Life Re-written
- Amnesia and identity
- Belfast Marathon
- Don't ignore the warning signs
- Dr Roger Weddell
- Helen Shaw – Headway South Cumbria
- Trevor Hall – Headway Hartlepool
- Alan McKnight - Finaghy volunteer
- A company-wide charity day in aid of Headway
- My pain monster
- Inspirational brain injury advocate Dr. Bruce Powell Joins Headway Charity Golf Day
- The Aphasia Theatre Group
- Caolan McCormick
- Liam Hamilton
- Let's go on holiday!
- Lasting Power of Attorney
- Peter's 3D model
- Headaches after brain injury: tips for Pain Awareness Month
- A journey from brain injury to the golf course with Headway
- Headway Cardiff's 1920s-inspired silent movie
- Author and brain tumour survivor has over 475,000 Facebook followers
- UK-based award-winning insurance company, Hastings Direct, steps forward for Headway
- Georgina's story
- Shopping without the stress after brain injury
- Connecting with nature after brain injury
- Martin’s Journey: Overcoming Intracranial Subdural Empyema
- Drained by fatigue? Try these 8 ways to cope after brain injury
- Menopause after brain injury
- Hosting or attending an event
- Elle's story: Life beyond post-concussion
- Steve Lightly
- Ataxia after brain injury
- The benefits of singing for brain injury survivors
- Concussion, head impacts and brain blood vessel function Q&A
- 10 reasons why you should join Eden's team in the Great North Swim
- Being seen and accepted after brain injury
- The Waiting Room a short film created by Headway Newtonabbey
- Q&A with Amarachi Nwaneri
-
For professionals
- Approved Provider scheme
- Criminal Justice System Professionals
- Events and conferences
- GPs
- Headway Head Injury Solicitors Directory
- Headway services
-
Headway webinars
-
Webinar recordings
- Life after acquired brain injury: Coping with anxiety and depression
- Smell and taste disorders after brain injury
- Fatigue after brain injury
- Managing sleep and fatigue after brain injury
- Nature’s benefit after brain injury
- Brain Injury in the Criminal justice System
- Managing memory problems after brain injury
- Identity change after brain injury
- Headway’s 2023 policy and public affairs round-up
- Disability discrimination in the workplace
- Understanding and responding to behaviours that challenge following acquired brain injury
- Moving towards digital care
- Mind the Gap: Navigating Social Care after Acquired brain Injury
- Covid and the brain: what we know so far
- Addiction and brain injury
- De-mystifying mental capacity
- Returning to work after brain injury
- Diet and nutrition after brain injury
- Head Injury and the Criminal Justice System in Scotland
- Understanding Personality Change After Brain Injury
- Post-traumatic Stress Disorder After Brain Injury
- Brain Blood Flow Regulation After Brain Injury
- Mental Health and Brain Injury
- Experiences and Challenges Faced by Family Members after Brain Injury
- Frontal Lobe Problems After Brain Injury
- Emotional Lability Following Brain Injury
-
Webinar recordings
-
Training courses
- Understanding MY brain injury
- Navigating life after brain injury
- An introduction to brain injury
- Understanding brain injury
- Effective communication strategies
- Understanding behaviours that challenge
- Goals setting training
- Brain Injury Solicitors training
- Understanding brain injury training for criminal justice professionals
- Headway group training sessions
- Further information
-
Featured
-

Stories of life after brain injury
Stories of life after brain injury
-
-
For individuals
-
Supporting you test
-
Supporting you
- In your area
- Helpline
- Brain Injury Identity Card
- Headway Emergency Fund
- Headway’s Justice Programme
- Online communities
- Keeping family and friends updated
- I recently sustained a brain injury
- I'm living with a brain injury
- Someone I know has a brain injury
-
Featured
-

Get support near you
Get support near you -

Legal advice
Legal advice -
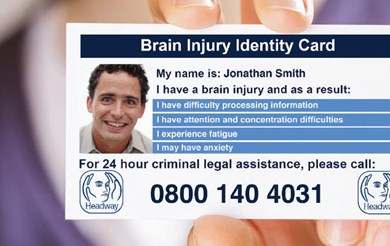
Brain Injury Identity Card
Brain Injury Identity Card
-
-
Supporting you
-
News and campaigns
- News and stories
- Campaigns
-
Featured
-
Headway News spring 2025
Headway News spring 2025 -
Budget for brain injury
Budget for brain injury
-
-
Get involved
-
Fundraise for us
- Hats for Headway Day
- Headway Charity Golf Day
- Virtual fundraising: Facebook Challenge
-
Take on a challenge
- Find your local event
-
Run, swim, cycle
- Amsterdam Half Marathon
- Barcelona Marathon
- Bath Half Marathon
- Brighton Marathon
- Cardiff Half Marathon
- Dorney Lakes Duathlon
- Edinburgh Marathon Festival
- Great Manchester Run 10K
- Great Manchester Run Half Marathon
- London 10k
- Great North Run Half Marathon
- Great North Swim Quiet Wave
- Great Scottish Run 10K
- Great Scottish Run Half Marathon
- Hackney Half Marathon
- London Landmarks Half Marathon
- London to Paris cycle ride
- Manchester Half Marathon
- Manchester Marathon
- Paris Half Marathon
- Paris Marathon
- Royal Parks Half Marathon
- TCS London Marathon
- Tough Mudder
- Ultra Challenge Series
- World famous marathons with realbuzz
- Yorkshire Marathon
- Treks and walks
- Skydives
- Corporate events
- Bungee jumps
- Friends of Headway
- Payroll Giving
- Organising your own event?
- Download your fundraising pack
- Easy ways to support us
- Headway Annual Awards
- Organisations
- Donate
- Volunteer with us
-
Fundraise for us
-
My story
- Brain injury and me
-
Featured
-

Brain injury and me
Brain injury and me -

Simon and Marc's story
Simon and Marc's story -

Nigel and Paula's story
Nigel and Paula's story
-
-
About Headway
-
Our organisation
-
Events and conferences
- Headway webinar series
- Headway training courses
- Hats for Headway Day
- Action for Brain Injury (ABI) Week
- Volunteers' Week
- Carers Week: Caring About Equality
- Hard Hat Awareness Week
- Headway Charity Golf Day
- Second Hand September
- Mince Pie Morning
- Headway Annual Awards
- Look Ahead in the North
- ABI Games 2025
- Neuroplasticity in Action conference 2025
- Aims and objectives
- The history of Headway
- Contact us
- Accounts
-
Events and conferences
- Working with us
- Shop with us
-
Featured
-

Help us continue our work
Help us continue our work
-
-
Our organisation





